Do I really owe this money?
Medical bills are a hassle. Sometimes we know it is a legitimate bill that needs to be paid. Sometimes it is unclear who the bill is from or why we are being charged. Sometimes, we don’t owe a dime because of timing issues, communication discrepancies, or just simply being the victim of some undesirable billing practices from 3rd party services.
I was shocked when one of our clients got up during an Open Enrollment meeting and let all of his employees know that if they got a bill in the mail for medical services to “assume the bill isn’t right–no matter what.” That was some shocking and unexpected advice, but time and time again that wisdom has proved right more often than it has been wrong. So, I now request of you, assume the bill is wrong and let’s dive into discovering if you owe money to a doctor or medical provider.
Does the bill match what your insurance says you owe?
If you have health insurance, each service you receive becomes a “claim”. Sometimes you owe 100% for that service, sometimes you owe zero, and sometimes you owe a portion. To understand what the bill says versus what the insurance says, you need to compare those two sources of information. If you have a bill from a doctor’s office, you should also have an “EOB” or Explanation of Benefits from your insurance company. Now, you may get those in the mail or they may be posted online in your Member Login.
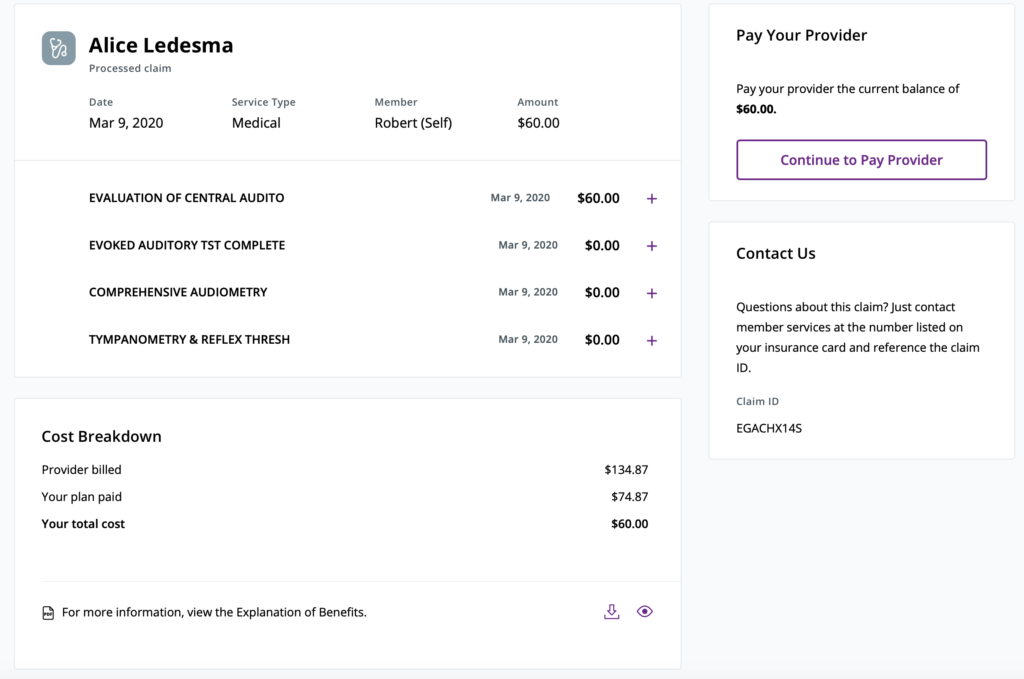
Wait, you haven’t created your Member Login yet? Don’t worry, today is the day to get started. And good news, these websites have become extremely user friendly and many keep a quick dashboard of what you owe or what you don’t owe. Some even have the ability to pay the correct amount you owe to the provider directly through your member portal. And, if you have one of the really cool and innovative plans, your insurance company might have already paid the bill on your behalf and negotiated the lowest amount for you in advance.
Back to reading that insurance statement that says what you owe
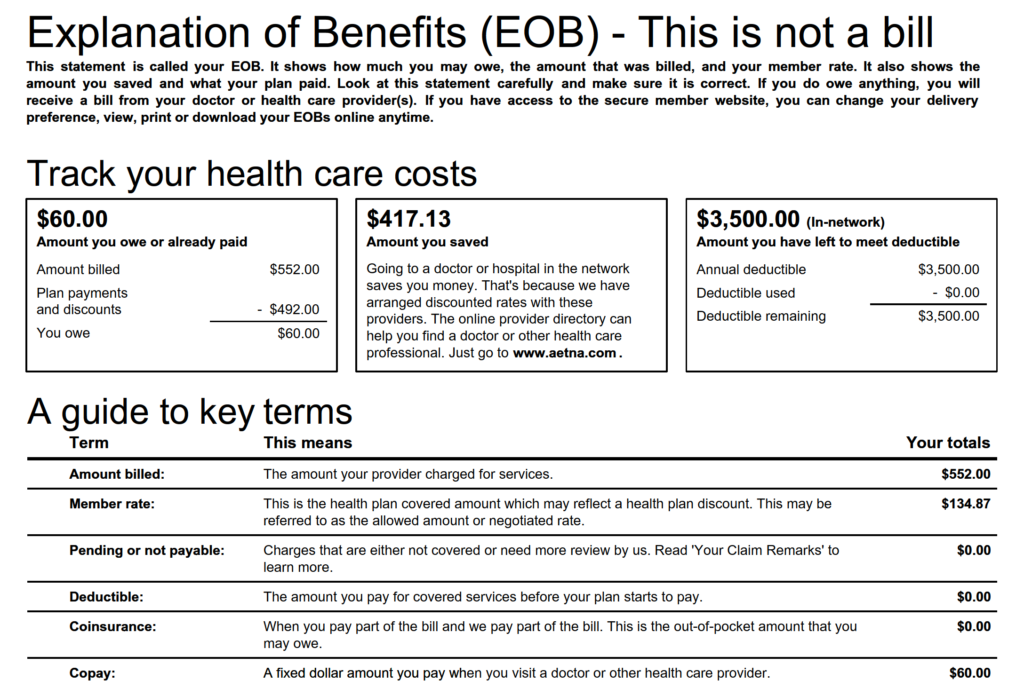
Each item that occurs during an appointment starts with a condition or diagnosis code, also known as an ICD-10 code. That code translates to a diagnosis and triggers a whole list of acceptable billing options for time and severity. Essentially, if a doctor bills for a flu test, it would only be appropriate if you showed symptoms. And thus, for most simple doctors visits you’ll see 2 or 3 lines of codes that equal a total “billed” charges. From that “billed charge”, you should see an “allowed amount”. This allowed amount is the price of the service based on the network contract that the doctor or their medical practice has agreed to with your insurer. Then, your plan assigns each of those allowed items to the insurance’s mathematical equations that get explained in cost-sharing terminology like Deductible, Co-Insurance, Copay, and the dreaded Not-Covered category. And, finally, each explanation gives you the total amount you owe.
Online View
Paper EOB
But my bill doesn’t match
If your bill from the doctor or other medical provider doesn’t match the total on the EOB, now we have a problem to work on.
First, check that the invoice from your medical service provider to see if there is a prior balance carried forward. Yes, unpaid bills that you didn’t know about are very common. The difference on the invoice they are sending you might be something from a prior service that needs more detail.
Next, review the dates of service to see if they expand beyond the scope of the EOB you are looking at. If so, you may need to go back to your insurance’s member portal and download or review those extra dates of service.
And, if they still don’t match, it is time to pick up the phone and call the billing company or see if that invoice has a payment portal listed. Often, there might even be a different amount listed on a billing service’s payment portal than your invoice, especially if your insurance has paid a portion of your claim after the date the provider’s billing service generated that invoice they sent to you.
*Please be aware, it is very common for your doctor’s office or other medical provider to have an outside billing service. So, the number on the bill or the payment portal may be completely different from your provider’s phone number or portal they provide for patient records.*
My invoice matches my EOB, but I disagree
Now this is where things get interesting. Sometimes when you look at that EOB or that invoice you’ll see services you don’t recall, tests you don’t recognize, or items you didn’t request. You may also just simply be appalled at the cost of a particular service you weren’t expecting.
For this level of resolving your bill, I want to let a couple of our partners who specialize in member advocacy give you some helpful tips that they use.
From our friends at the former Medibookr
You’ll want to identify how the claim actually processed that has yielded higher than expected out-of-pocket costs. Pay close attention to identify if the provider sending you the bill was “In-Network” or “Out-of-Network”.
If the bill was processed as out-of-network, but the provider is actually in-network:
Contact your insurance company’s member services line and ask for an explanation to find out what portion of a claim that was filed caused it to process out-of-network.
Then, work with your provider’s billing office to get a corrected claim submitted to your insurance so that it will process as In-Network. This generally has to do with claim being submitted with an incorrect tax ID or National Provider Information (NPI number) combination.
If the bill processed out-of-network, but is part of an in-network claim:
If you visit an In-Network provider and there are services performed by other providers who do not participate in the same network, call your insurance company’s member services and explain that the provider billing you was associated with an In-Network service. Request to have their bills also processed at the In-Network level of benefits at the usual and customary rate (UCR). Once processed at the in-network level of benefits, you will need to work with medical billing office and request that they accept the reprocessed payment from your insurance at In-Network or UCR amounts as payment in full, and verify that they will not balance bill the remaining portion of submitted charges.
You can call and request a cash-pay amount or prompt-pay amount where the Out-of-Network provider will accept a reduced rate to immediately resolve the amount. Verify this payment will result in an agreement to not balance bill the remaining portion of the originally submitted charges.
If the bill processed out-of-network, but was a true medical emergency:
You will need to work directly with your insurance company’s claims processor at first and explain the emergency situation and have it processed at the In-Network rate.
Typically in an emergency, these services fall under ERAP clauses that also protect against out of network charges.
Tips that apply in any situation:
If a provider is being unreasonable and you feel there are egregious charges, formal complaints can be made to both TDI (Texas department of insurance) and various state departments.
Some employers sponsor a Self-Insured or ERISA qualified arrangement. In this scenario, many of the Third Party Administrators (TPAs) who process your claims have a specific negotiation department that actually works to proactively negotiate balance billing and out-of-network charges at a lower more reasonable rates.
Finally, please note that once you start an appeal with your health plan, that once things get to 2nd and 3rd level appeals, insurance rulings are final. That is why it is always best to appeal and plead with provider’s office or billing company first.
Next, from our friends at freshbenies
We really believe in outsourcing this process.
- Advocates review bills for accuracy, negotiate reductions, and research and resolve claim denials. Employees benefit from not having to deal with complicated medical bills and the savings that comes from an expert review. Employers get the benefit of maintaining stronger productivity levels — including hours of saved HR efforts.
- Advocates are an independent resource. When advocacy services are separate from the health plan, employees have confidence that referrals, bill negotiations and overall guidance are not influenced by outside factors.
- Advocates work with providers and carriers on the member’s behalf to resolve errors or overcharges. Based on actual claims-verified savings between the original amount owed and the reduced outstanding patient portion.
So how does someone get started with outsourcing this headache to an advocate?
- To get started, the member simply emails or faxes a copy of their bill(s) to their Advocate for review.
- The Advocate will then review the bill by contacting the member’s insurance company and the provider’s office to make sure the bill was processed correctly and that the In-Network benefits were applied.
- If there are any billing issues along the way (like the bill needs to be re-coded, re-processed or appealed OR the member needs a refund), the Advocate will resolve those issues for the member.
In the end, all of the time a member would’ve spent waiting on hold, dealing with different provider offices, calling the insurance company, and following-up are taken care of by their Advocate. No bill is too big or too small for review, so members just need to send them on over!


